Number: 116-24
Date: December 9, 2020
House Passes H.R. 2477, the “BENES Act of 2020”
On December 8, 2020, the House passed H.R. 2477, the Beneficiary Enrollment Notification and Eligibility Simplification Act of 2020 (BENES Act of 2020), as amended, under suspension of the rules. The bill now moves to the Senate for consideration.
This bill includes the following provisions of interest to the Social Security Administration (SSA):
Medicare Outreach Notices
- Would require the Centers for Medicare and Medicaid Services (CMS) to develop a Medicare outreach notice, in consultation with SSA and various stakeholder groups. The notice would include information on the following topics:
- eligibility for Medicare benefits, in particular Parts B and C;
- the penalties for not enrolling in Medicare timely and how the penalties are calculated;
- the circumstances under which a person could enroll without penalty or receive relief from those penalties;
- the need for coordination of benefits under Part B;
- special considerations for certain populations, including residents of Puerto Rico and veterans; and
- information on the online resources provided by CMS and SSA and the agencies’ toll free numbers.
- Would require SSA to:
- post the outreach notice on our public website;
- include the outreach notice with the Social Security Statement we provide to individuals who are attaining age 63, 64, and 65; and
- send the outreach notice to the following people two times around the end of their waiting period for Medicare:
- disability beneficiaries (including disabled widows and people who receive childhood disability benefits);
- Railroad Retirement Board disability beneficiaries; and
- certain Medicare-qualified government employees.
- Would require CMS to reimburse SSA from the Medicare Trust Funds for the cost of our activities related to the outreach notices. We could use our administrative appropriation (the “Limitation on Administrative Expenses”) to temporarily fund the work needed to establish the agreement and for work necessary to implement the outreach notice prior to establishment of the agreement.
- Would be effective two years after the date of enactment.
Earlier Coverage after Enrollment in an IEP or GEP
Authority for HHS to Establish SEPs for Exceptional Circumstances
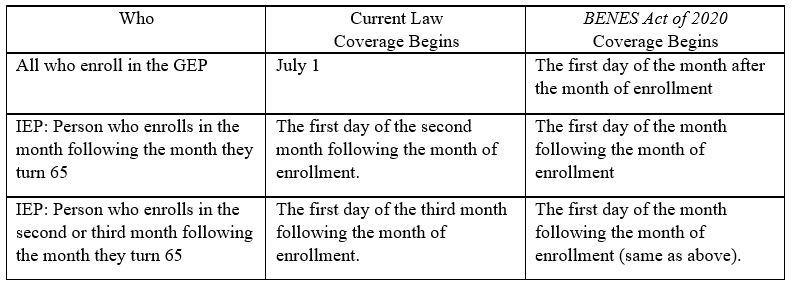
- Would make Medicare coverage take effect earlier for people who enroll in the General Enrollment Period (GEP) or the last three months of their Initial Enrollment Period (IEP), as follows:
- Would authorize the Secretary of Health and Human Services to establish a special enrollment period for people in exceptional circumstances, as defined by the Secretary.
- Would be effective January 1, 2023.
Extended Coverage of Immunosuppressive Drugs for Kidney Transplant Patients
- Enrollment in Parts A and B for people who have end-stage renal disease generally ends 36 months after they receive a successful organ transplant. This bill would allow a person who has no other health insurance coverage to remain enrolled in Part B beyond this period for the purpose of covering immunosuppressive drugs
- The premium for this extended Part B coverage would not be subject to late enrollment penalties and would be less than the standard Part B premium.
- Coverage would start January 2023, as follows:
- People whose 36-month coverage period ends before January 2023 could enroll starting in October 2022 and their coverage would start the later of January 2023 or the month after they enroll; and
- o People whose 36-month coverage period ends January 2023 or later would be automatically enrolled.